Hip Replacement
What is a total hip replacement?
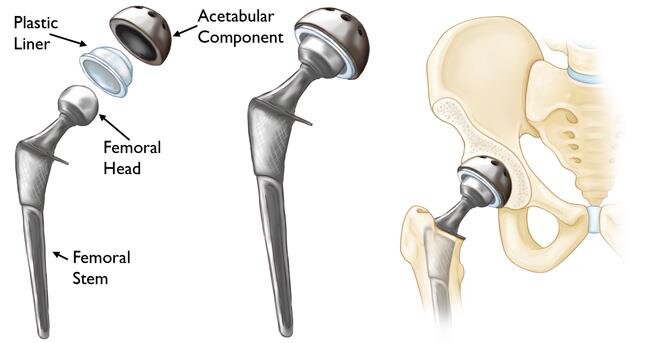
A total hip replacement is an operation in which the damaged hip joint is removed and replaced with a prosthetic implant. This is made up of four main parts; the femoral stem, the acetabular cup (socket), the socket liner and the ball. Since it was first performed in 1960, hip replacement has become one of the most successful operations ever invented. Hip replacement surgery is a safe and effective procedure that can relieve your pain, increase range of motion, and help you to enjoy everyday activities.
What conditions can be treated with a hip replacement?
A hip replacement is the surgical solution for a large number of conditions which can affect the hip joint. These include:
Osteoarthritis
Inflammatory or rheumatoid arthritis
Avascular necrosis
Hip dysplasia.
Hip replacement surgery is only indicated when appropriate non-surgical treatment is no longer effective. Mr Gormack will assess your individual circumstances and can advise whether hip replacement is the right option for you. To learn more about these hip conditions refer to our hip conditions page.
How is the surgery done?
Most of the time the hip replacement operation is done under spinal anaesthetic. This involves a small injection in your back that will make the lower half of your body completely numb for approximately four hours. After the injection (spinal) is done you will lie on your side. If you would prefer to be asleep for your surgery you will be given medication through a drip in your arm to make you sleep. The operation will take approximately 90 minutes. An incision is made over your upper thigh, the old hip joint is removed and the new implants are fitted into your hip joint. The skin is then closed with dissolving stitches. Dressings are put on, including paper stitches (steri-strips) and a waterproof dressing. You will be moved onto a comfortable bed and taken to the recovery area to wake up under observation. While you are in the recovery area, an x-ray will be taken of your new hip joint.
What type of Hip implant will be used?
There are many different types of hip implant, and each implant comes in a range of sizes. Choosing the best implant for you will depend on a number of factors. Mr Gormack will take into account your age, the size and shape of your bones, whether you have osteoporosis, and your expected activity levels after surgery. In general, cemented implants will be used in patients with wider or thinner (osteoporotic) bone, and uncemented implants will be used in patients with harder or thicker bone. The socket is made of titanium, with a liner made from a plastic called ‘highly cross-linked polyethelene’. The stem that goes inside the thigh bone is stainless steel or titanium, and the ball is made from either stainless steel or ceramic. Before surgery you will have a templating x-ray to ensure the correct size and shape implant is selected for you.
What APproach will be used?
The particular method that a surgeon uses to perform surgery is called the approach. There are many different surgical approaches used to perform total hip replacement. Each method has its own advantages and disadvantages. The approach used by your surgeon is determined by their training and experience, as well as the individual anatomy of your hip joint. Some approaches can allow slightly faster early recovery after surgery, but after the first six weeks there will be no noticeable difference. Mr Gormack uses one of three different approaches:
The conventional posterior approach
This involves a scar over the buttock and upper leg. This is the approach used by most hip surgeons in New Zealand and gives very reliable results. This approach gives the best access for complex cases, or in very large or muscular patients.
The direct superior approach
This is a minimally invasive version of the posterior approach. The scar is smaller and the amount of muscle damage internally is less than the posterior approach. Recovery is generally faster with less pain and a lower risk of dislocation. Mr Gormack uses this for the majority of hip replacements.
The direct anterior approach
This approach involves a scar over the front of the hip. Early recovery is faster with less pain, and a lower risk of dislocation. The operation is more technically challenging than alternative approaches . It is currently not suitable for all patients.
WHAT should i do before surgery?
The results of surgery are dependent on both the operation done by your surgeon, but also your health and wellness prior to the operation. Making the following changes to your lifestyle will give you the best possible outcome from your surgery:
Reduce or quit smoking. Smoking slows wound healing and increases your risks of infection after surgery. Ask your GP for help or call Quitline on 0800 778 778.
Reduce alcohol intake. Alcohol can have an affect on the medications used during your surgery, and can increase the risk of confusion after surgery.
Continue regular exercise. Daily low impact exercise improves your overall fitness and maintains muscle strength. This will help you rehabilitate more quickly after surgery. Cycling, swimming and walking (if tolerated) are all good ways to stay fit.
Stay on top of your pain. Take regular simple pain medication such as paracetamol or celecoxib (Celebrex). This will allow you to sleep comfortably and maintain regular exercise until your surgery date.
Choose mainly healthy foods to eat. A balanced diet with lots of fruit, vegetables and lean protein will improve your recovery and healing after surgery. Cut down on fast foods, treats and sugary drinks.
See your dentist. Broken or damaged teeth can be a source of infection in your bloodstream, which can get into your new hip joint. These should be treated at least a week prior to your surgery.
Get your diabetes under control:
o Poorly controlled diabetes is one of the biggest risks for infection after your hip replacement. High blood sugars help infection grow.
o Keeping tight control of your blood sugar levels for weeks or ideally months before surgery is needed to reduce your risk.
o Your GP can check your long-term blood sugar control with a blood test called HbA1C. Ideally this should be below 55.
Treat iron deficiency anaemia. If you are anaemic (low in iron) before surgery you have a higher risk of needing a blood transfusion. Eating lean red meat regularly helps to improve iron levels if you are low. Occasionally iron tablets are required. If in doubt see your GP for a simple blood test.
Lose some weight if you are overweight. Being overweight increases the risk of infection after surgery, and makes rehabilitation harder. Even small amounts of weight loss are helpful and worthwhile.
What is the recovery after surgery?
After surgery is complete, you will be taken to a ward in another part of the hospital. If you have had a spinal anaesthetic your legs will stay numb for another 2-3 hours. You can eat and drink normally as soon as you feel ready. Your nurse will monitor your pulse, blood pressure and oxygen levels and provide you with pain relief and anti-nausea medication as required. It is better to keep on top of pain instead of trying to be tough. You will have foot pumps on your feet to help keep your circulation moving and prevent blood clots in your legs. Moving your feet regularly yourself is also helpful. You will soon be encouraged to get out of bed and start walking. A physiotherapist will help you the first time you stand up. Most patients are able to stand and even walk a few steps on the same day as surgery. It is very common to feel a bit faint or dizzy the first time you stand up after your operation. The average stay in hospital is around 2-3 nights after surgery and Mr Gormack will check on you each day while you are in hospital. A physiotherapist will see you daily, and teach you how to walk with a frame or crutches. They will also give you exercises to do yourself. Once you are confident that you can walk around and do your daily activities independently, you will be able to go home. Before you go, you will also be given advice on how to avoid a hip dislocation.
It generally takes around six weeks to fully recover from surgery. You will be able to gradually increase walking distance and duration over this time. You can stop using crutches when you feel confident and steady on your feet. For most people this takes 2-4 weeks. Sometimes a single crutch is helpful when walking outdoors for longer periods. You will need to have your wound checked 10 – 14 days after surgery. This can be done at Mr Gormack’s clinic, or by your own GP depending on what is most convenient for you. Pain levels will steadily decrease. You should aim to stop taking strong pain relief such as tramadol or oxycontin within two weeks of surgery. Paracetamol or ibuprofen can be continued as needed for up to six weeks. You will have an appointment booked to see Mr Gormack approximately six weeks after your surgery. If you have any urgent concerns prior to this appointment, please call or email the clinic.
What are the risks of surgery?
There are risks associated with any surgery. Modern hip replacement is a very safe and successful operation, and the chance of having a significant problem are very low. The main risks of surgery include:
Infection
Bleeding
Nerve damage
Blood clots in the legs or lungs (DVT / PE)
Dislocation
Fracture
Leg length difference
Medical events after surgery such as heart attack, kidney injury, stroke, or pneumonia.
What activities can I do / not do after surgery?
You will be able to gradually increase your activity level as you recover from surgery. You can walk on your new hip immediately after surgery, and stop using crutches as soon as you feel confident. Increase your walking distances over the next few months. You can start swimming and using an exercise bike after six weeks, and resume outdoor cycling after 8-12 weeks. With time you should be able to return to a full active lifestyle including regular walking, sporting activities such as golf, tennis, cycling and skiing. While it is possible to run on your new hip, regular jogging is not recommended as this can cause premature wear and tear of the implants. While excellent range of motion is possible after hip replacement, it is safest to avoid extreme movements such as deep squatting, twisting or sitting cross-legged on the floor.
When can I drive?
In order to drive safely you need to be able to control your vehicle and react quickly in the event of an emergency. For most people, this takes around six weeks after hip replacement surgery. If you have had a left hip replacement and drive an automatic car, driving may be possible after four weeks. If you drive too early after surgery you may not be covered by your insurance provider and may be liable in the case of an accident.
When can I return to work?
Every job is different, so returning to work depends on the particular physical requirements of your job. Most people will take around six weeks to return to work, although occasionally those with a sedentary occupation may return to work earlier. People with jobs that require a lot of standing and walking may take 8 - 12 weeks to return to work. If your job is very physically demanding then it may take 3 - 6 months to return to full duties, although light duties are generally possible earlier than this. Mr Gormack can give you a more specific estimate based on your individual circumstances.
How long will my hip replacement last?
Modern hip replacement implants are very durable, and generally last a long time. In New Zealand over 90% of hip replacements will last more than 10 years, and over 70% will last more than 20 years. Your age, size and activity level will determine how long your new hip will last. If you are over 65 years old when you have a hip replacement, there is a very high chance that this will last for the rest of your life. If you are very young, or place excessive load on your implants from heavy physical activity or excessive weight, your hip implant may not last as long. If your hip replacement wears out it is usually possible for it to be revised (redone). Revision surgery is often challenging, and the results of a revision hip surgery are seldom as good as the first one.
Will I set off metal detectors at the airport?
Hip replacement implants are mainly metal. This means that they will set off the metal detectors at most airports. As hip replacement surgery is very common, airport security staff are accustomed to seeing people with artificial joints. There is no need to carry documentation with you; simply tell the airport security staff that you have an artificial hip, and they will confirm this with a hand held scanner.